Did you know that the incidence of primary liver cancer has more than tripled since 1980?
More than 40,000 Americans will be diagnosed with primary liver cancer this year, according to the American Cancer Society. And thousands of others will be diagnosed with secondary (metastatic) liver cancer, cancer that spreads to the liver after starting somewhere else in the body.
While surgery remains the gold standard for treating liver cancer, advances in medicine have made more treatment options available, especially for patients who may not be able to tolerate surgery or in cases where tumors are too large to be removed safely.
At the Edward & Marie Matthews Cancer Center at University Medical Center of Princeton, patients have access to a full range of services for the diagnosis and treatment of cancer, including liver cancer.
Liver Basics
Your liver is your largest internal organ and is positioned under your right ribs just beneath your right lung. It consists of two lobes, and weighs a total of about 3 pounds. It is also unique in that it has two blood supplies — the portal vein and the hepatic artery.
Your liver performs many vital functions including removing toxins from your blood, breaking down and storing nutrients that power your body and repair tissues, and producing bile to help your body absorb nutrients.
Many primary liver cancers are related to the hepatitis B or hepatitis C virus, which increase the risk for liver cancer. Other common risk factors include:
Gender. More men develop liver cancer than women.
Cirrhosis. A disease that causes scarring of the liver and is most associated with alcohol abuse and hepatitis, cirrhosis increases the risk for liver cancer.
Diabetes. Type 2 diabetes has been linked with an increased risk of liver cancer, usually in patients who have other risk factors such as heavy alcohol use, chronic viral hepatitis, or a combination of the two.
Obesity. Obesity can increase the risk for liver cancer as it is associated with diabetes as well as non-alcoholic fatty liver disease, which can lead to cirrhosis.
In addition, liver cancer can also be caused by other cancers that have started elsewhere in the body and metastasized to the liver. Metastatic liver cancer is most commonly associated with colon, lung and breast cancer.
Advances in Treatment
Traditional treatment for liver cancer typically involves surgery, chemotherapy and external beam radiation.
However, not all patients are candidates for surgery and some may not respond to traditional chemotherapy and radiation.
Today, there are several innovative approaches — such as radioembolization, chemoebolization and microwave ablation — that are making treatment more precise and more accessible to a broader number of patients.
With radioembolization, radiologists insert a catheter into the hepatic artery — the blood supply to the tumor — and insert tiny beads that lodge in the artery and give off small amounts of radiation, selectively targeting the tumor.
The procedure, which is performed through a small incision in the groin or the wrist and guided by X-ray images, kills the cancer cells and shrinks the tumor while sparing the surrounding healthy liver tissue.
Radioembolization is a generally a treatment option for cancer that is largely confined to the liver and for patients who meet certain baseline standards for liver function.
Similar to radioembolization, chemoembolization uses a catheter in the hepatic artery to delivery tiny beads of chemotherapy to the tumor. It is most beneficial in patients whose cancer is predominately limited to the liver.
Both radioembolization and chemoembolization block or reduce blood flow to the tumor, helping to kill off the cancer cells. Because the main blood supply to the liver is through the portal vein, healthy liver cells are relatively unharmed.
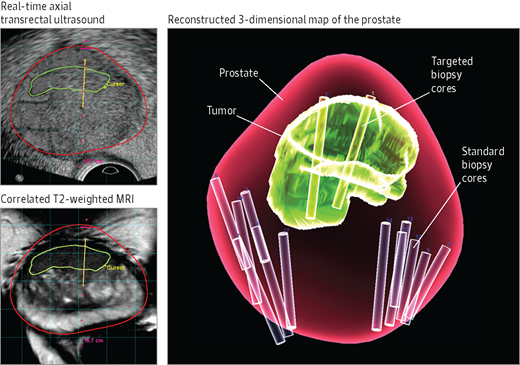
Another procedure, microwave ablation uses heat to destroy tumors. With microwave ablation, doctors — guided by an ultrasound or CT scan — insert a needle-like probe into the tumor. The probe emits heat from microwave energy that reaches temperatures greater than 100 degrees and kills the cancer cells.
Microwave ablation is typically used to treat smaller tumors, generally no more than 2 inches across.
All three procedures are generally well tolerated by patients. Side effects are typically mild and may include low-grade fever, abdominal pain and nausea. Usually, the procedures are performed on an outpatient basis.
In addition, because the procedures are precisely targeted there is normally little damage to healthy liver cells.
An Individualized Approach
As with most diseases, there is no single right approach for treating liver cancer. Each patient is different and requires a treatment plan that is specific and targeted to their unique condition.
Fortunately, innovations in cancer care are enabling doctors to manage complex cancer cases with more precise treatment, ultimately providing better outcomes for their patients.
If you have been diagnosed with liver cancer, talk with your doctor about your treatment options and the safest and most effective approach for your individual condition.
The Edward and Marie Mathews Cancer Center at UMCP is accredited with commendation from the American College of Surgeons’ Commission on Cancer and a recipient of the American College of Surgeons’ Commission on Cancer Outstanding Achievement Award. UMCP and the UMCP Breast Health Center earned accreditation from the National Accreditation Program for Breast Centers, and the UMCP Breast Health Center is designated as a Breast Imaging Center of Excellence by the American College of Radiology.
This article was written by our own Samuel J. Greene, M.D. and originally published on CentralJersey.com.